Caterack Removal
| Cataract surgery | |
|---|---|
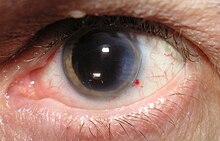
 Magnified view of a cataract in a human eye seen on examination with a slit lamp | |
| Specialty | Ophthalmology |
| ICD-ix-CM | 13.19 |
| MeSH | D002387 |
| MedlinePlus | 002957 |
Cataract surgery, also chosen lens replacement surgery, is the removal of the natural lens of the eye (also called "crystalline lens") that has developed an opacification, which is referred to as a cataract,[i] and its replacement with an intraocular lens. Metabolic changes of the crystalline lens fibers over fourth dimension pb to the development of the cataract, causing damage or loss of vision. Some infants are born with congenital cataracts, and certain environmental factors may also atomic number 82 to cataract formation. Early symptoms may include strong glare from lights and pocket-sized light sources at nighttime, and reduced vigil at low lite levels.
During cataract surgery, a patient's cloudy natural cataract lens is removed, either by emulsification in identify or by cut it out. An bogus intraocular lens (IOL) is implanted in its place. Cataract surgery is generally performed past an ophthalmologist in an convalescent setting at a surgical center or hospital rather than an inpatient setting. Either topical, sub-tenon, peribulbar, or retrobulbar local anesthesia is used, commonly causing little or no discomfort to the patient.[two]
Well over ninety% of operations are successful in restoring useful vision, with a low complication rate. Mean solar day intendance, loftier volume, minimally invasive, small incision phacoemulsification with quick post-op recovery has become the standard of care in cataract surgery all over the world.
Types [edit]
Ii principal types of surgical procedures are in common use throughout the world. The first process is phacoemulsification (phaco) and the 2d involves 2 different types of extracapsular cataract extraction (ECCE). In most surgeries, an intraocular lens is inserted. Foldable lenses are generally used for the 2–three mm phaco incision, while not-foldable lenses are placed through the larger extracapsular incision. The pocket-size incision size used in phacoemulsification (2–3 mm) ofttimes allows "sutureless" incision closure. ECCE uses a larger incision (x–12 mm) and therefore usually requires stitching, and this in part led to the modification of ECCE known as manual small incision cataract surgery (MSICS).
Cataract extraction using intracapsular cataract extraction (ICCE) has been superseded by phacoemulsification and ECCE, and is rarely performed.
Phacoemulsification is the most normally performed cataract procedure in the adult world. However, the loftier cost of a phacoemulsification car and of the associated disposable equipment means that ECCE and MSICS remain the most commonly performed process in developing countries.
Cataract surgery is commonly done every bit twenty-four hours intendance rather than in-patient procedure as there is some evidence that 24-hour interval surgery has like outcomes and is cheaper than hospitalisation and overnight stay.[3]
Types of surgery [edit]

Cataract surgery, using a temporal approach phacoemulsification probe (in right hand) and "chopper" (in left hand) being done under the operating microscope at a Usa Navy medical center
Cataract surgery recently performed, foldable IOL inserted. A small-scale incision and very slight hemorrhage are visible to the right of the still dilated student.
At that place are a number of different surgical techniques used in cataract surgery:
- Phacoemulsification (phaco) is the nigh common technique used in adult countries. Information technology involves the employ of a machine with an ultrasonic handpiece equipped with a titanium or steel tip. The tip vibrates at ultrasonic frequency (xl,000 Hz) and the lens textile is emulsified. A second fine musical instrument (sometimes chosen a "cracker" or "chopper") may be used from a side port to facilitate cracking or chopping of the nucleus into smaller pieces. Fragmentation into smaller pieces makes emulsification easier, besides as the aspiration of cortical material (soft part of the lens around the nucleus). Afterward phacoemulsification of the lens nucleus and cortical cloth is completed, a dual irrigation-aspiration (I-A) probe or a bimanual I-A system is used to aspirate out the remaining peripheral cortical material.
- Manual modest incision cataract surgery (MSICS): This technique is an evolution of ECCE (see beneath) where the unabridged lens is expressed out of the eye through a self-sealing scleral tunnel wound. An appropriately constructed scleral tunnel is watertight and does not crave suturing. The "minor" in the title refers to the wound being relatively smaller than an ECCE, although it is still markedly larger than a phaco wound. Head-to-head trials of MSICS vs phaco in dense cataracts have constitute no divergence in outcomes, simply shorter operating time and significantly lower costs with MSICS.[ medical citation needed ]
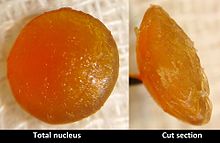
Nucleus of hypermature cataract afterward ECCE
- Extracapsular cataract extraction (ECCE): Extracapsular cataract extraction involves the removal of virtually the unabridged natural lens while the elastic lens capsule (posterior capsule) is left intact to allow implantation of an intraocular lens.[four] It involves manual expression of the lens through a big (usually 10–12 mm) incision made in the cornea or sclera. Although it requires a larger incision and the use of stitches, the conventional method may be indicated for patients with very hard cataracts or other situations in which phacoemulsification is problematic.
- Intracapsular cataract extraction (ICCE) involves the removal of the lens and the surrounding lens capsule in 1 piece. The procedure has a relatively loftier rate of complications due to the large incision required and pressure placed on the vitreous torso. It has therefore been largely superseded and is rarely performed in countries where operating microscopes and high-technology equipment are readily available.[4] Afterward lens removal, an artificial plastic lens (an intraocular lens implant) tin be placed in either the anterior bedroom or sutured into the sulcus.
- Femtosecond light amplification by stimulated emission of radiation-assisted cataract surgery has been shown to have no visual, refractive or safety do good over transmission phacoemulsification.[5] [half-dozen]
Cryoextraction is a form of ICCE that freezes the lens with a cryogenic substance such as liquid nitrogen.[vii] In this technique, the cataract is extracted through use of a cryoextractor – a cryoprobe whose refrigerated tip adheres to and freezes tissue of the lens, permitting its removal. Although it is now used primarily for the removal of subluxated lenses, it was the favored grade of cataract extraction from the late 1960s to the early 1980s.[8]
Intraocular lenses [edit]
- Intraocular lens (IOL) implantation: Afterwards the removal of the cataract, an IOL is commonly implanted into the heart, either through a small incision (ane.eight mm to 2.eight mm) using a foldable IOL, or through an enlarged incision, using a poly(methyl methacrylate) (PMMA) lens. The foldable IOL, made of silicone or acrylic cloth of appropriate power is folded either using a holder/folder, or a proprietary insertion device provided along with the IOL. The lens implanted is inserted through the incision into the capsular bag within the posterior chamber (in-the-bag implantation). Sometimes, a sulcus implantation (in front or on top of the capsular bag but behind the iris) may be required because of posterior capsular tears or because of zonulodialysis. Implantation of posterior bedroom IOL (PCIOL) in patients below 1 year of age is controversial due to rapid ocular growth at this historic period and the excessive corporeality of inflammation, which may be very hard to command. Optical correction in these patients without intraocular lens (aphakic) is ordinarily managed with either special contact lenses or glasses. Secondary implantation of IOL (placement of a lens implant equally a second operation) may exist considered afterwards. New designs of multifocal intraocular lens are now available. These lenses let focusing of rays from distant also every bit virtually objects, working much like bifocal or trifocal eyeglasses. Preoperative patient option and proficient counselling is extremely important to avoid unrealistic expectations and post-operative patient dissatisfaction. Acceptability for these lenses has become better and studies have shown good results in selected patients.
In addition, there is an accommodating lens that was approved past the U.s.a. FDA in 2003 and fabricated by Eyeonics,[9] at present Bausch & Lomb. The Crystalens is on struts and is implanted in the heart's lens capsule, and its design allows the lens' focusing muscles to move it back and along, giving the patient natural focusing ability.
Artificial intraocular lenses (IOLs) are used to supercede the heart's natural lens that is removed during cataract surgery. These lenses have been increasing in popularity since the 1960s, simply information technology was non until 1981 that the first U.S. Food and Drug Assistants (FDA) approving for this blazon of product was issued. The development of IOLs brought about an innovation every bit patients previously did not take their natural lens replaced and every bit a upshot had to wear very thick eyeglasses or some special blazon of contact lenses. Before long,[ when? ] IOLs are peculiarly designed for patients with different vision problems. The main types of IOLs that at present exist are divided into monofocal and multifocal lenses.

A cataract surgery. Dictionnaire Universel de Médecine (1746–1748).
The monofocal intraocular lenses are the traditional ones, which provide vision at i distance merely: far, intermediate, or most. Patients who cull these lenses over the more developed types will probably need to article of clothing eyeglasses or contact lenses for reading or using the figurer. These intraocular lenses are ordinarily spherical, and they have their surface uniformly curved.[ medical citation needed ]
The multifocal intraocular lens is one of the newest types of such lenses. They are ofttimes referred to as "premium" lenses considering they are multifocal and accommodative, and allow the patient to visualize objects at more than i altitude, removing the need to wear eyeglasses or contact lenses. Premium intraocular lenses are those used in correcting presbyopia or astigmatism. Premium intraocular lenses are more expensive and are typically not covered, or not fully covered, by health insurance, every bit their boosted benefits are considered a luxury and not a medical necessity. An accommodative intraocular lens implant has only 1 focal point, but it acts as if it is a multifocal IOL. The intraocular lens was designed with a swivel like to the mechanics of the eye's natural lens.[ medical citation needed ]
The intraocular lenses used in correcting astigmatism are called toric, and accept been FDA approved since 1998. The STAAR Surgical Intraocular Lens was the first such lens developed in the The states and it may correct up to iii.5 diopters. A dissimilar model of toric lenses was created by Alcon and may correct upwards to 3 diopters of astigmatism. In order to attain the most do good from a toric lens, the surgeon must rotate the lens to exist on axis with the patient's astigmatism. Intraoperative wavefront assay, such as that provided by the ORA System developed past Wavetec Visions Systems, can be used to assist the doctor in toric lens placement and minimize astigmatic errors.[ medical citation needed ]
Cataract surgery may be performed to correct vision issues in both eyes, and in these cases, patients are usually advised to consider monovision. This procedure involves inserting in one eye an intraocular lens that provides near vision and in the other center an IOL that provides distance vision. Although most patients tin can adjust to having implanted monofocal lenses in both optics, some cannot and may feel blurred vision at both nearly and far distances. IOLs that emphasize distance vision may exist mixed with IOLs that emphasize intermediate vision in gild to accomplish a type of modified monovision. Bausch and Lomb developed in 2004 the first aspheric IOLs, which provide better contrast sensitivity by having their periphery flatter than the heart of the lens. Nonetheless, some cataract surgeons have questioned the benefits of aspheric IOLs, because the contrast sensitivity benefit may non last in older patients.[ medical commendation needed ]
Some of the newly launched IOLs are able to provide ultraviolet and bluish light protection. The crystalline lens of the centre filters these potentially harmful rays and many premium IOLs are designed to undertake this task as well. According to a few studies though, these lenses have been associated with a subtract in vision quality.[ citation needed ]
Another type of intraocular lens is the light-adjustable 1 which is still[ when? ] undergoing FDA clinical trials. This item blazon of IOL is implanted in the eye and and so treated with low-cal of a certain wavelength in order to alter the curvature of the lens.
In some cases, surgeons may opt for inserting an additional lens over the already implanted one. This blazon of IOLs procedures are chosen "piggyback" IOLs and are usually considered an option whenever the lens outcome of the starting time implant is not optimal. In such cases, implanting another IOL over the real 1 is considered safer than replacing the initial lens. This approach may also be used in patients who need loftier degrees of vision correction.
No thing which IOL is used, the surgeon will demand to select the advisable power of IOL (much like an eyeglass prescription) to provide the patient with the desired refractive outcome. Traditionally, doctors utilise preoperative measurements including corneal curvature, axial length, and white to white measurements to estimate the required power of the IOL. These traditional methods include several formulas including Hagis, Hoffer Q, Holladay 1, Holladay 2, and SRK/T, to name a few. Refractive results using traditional power calculation formulas leave patients within 0.5D of target (correlates to 20/25 when targeted for distance) or meliorate in 55% of cases and inside 1D (correlates to 20/40 when targeted for distance) or amend in 85% of cases. Contempo developments in interoperative wavefront technology such as the ORA System from Wavetec Vision Systems, have demonstrated in studies, ability calculations that provide improved outcomes, yielding 80% of patients within 0.5D (20/25 or better).
Statistically, cataract surgery and IOL implantation seem to be procedures with the safest and highest success rates when it comes to eye care. Withal, as with any other blazon of surgery, it implies certain risks. The cost is another important aspect of these lenses. Although most insurance companies cover the costs of traditional IOLs, patients may demand to pay the price difference if they cull the more than expensive premium ones.
Preoperative evaluation [edit]
An eye examination or pre-operative evaluation by an center surgeon is necessary to ostend the presence of a cataract and to determine if the patient is a suitable candidate for surgery. The patient must fulfill certain requirements such equally:
- The degree of reduction of vision due, at least in large office, to the cataract should be evaluated. While the existence of other sight-threatening diseases, such equally historic period-related macular degeneration or glaucoma, does not preclude cataract surgery, less improvement may be expected in their presence.
- The eyes should have a normal pressure, or whatever pre-existing glaucoma should exist adequately controlled with medications. In cases of uncontrolled glaucoma, a combined cataract-glaucoma procedure (phaco-trabeculectomy) can be planned and performed.
- The pupil should exist fairly dilated using eyedrops; if pharmacologic pupil dilation is inadequate, procedures for mechanical pupillary dilatation may be needed during the surgery.
- The patients with retinal disengagement may be scheduled for a combined vitreo-retinal procedure, along with PC-IOL implantation.
- In addition, information technology has recently been shown that patients taking tamsulosin (Flomax), a common drug for enlarged prostate, are prone to developing a surgical complication known as intraoperative floppy iris syndrome (IFIS), which must be correctly managed to avoid the complexity posterior capsule rupture; however, prospective studies accept shown that the risk is greatly reduced if the surgeon is informed of the patient's history with the drug beforehand, and has appropriate alternative techniques prepared.[x]
- A Cochrane Review of 3 randomized clinical trials including over 21,500 cataract surgeries examined whether routine preoperative medical testing resulted in a reduction of adverse events during surgery. Results showed that performing preoperative medical testing did not result in a reduction of risk of intraoperative or postoperative medical agin events, compared to surgeries with no or limited preoperative testing.[eleven]
Operation procedures [edit]
The surgical process in phacoemulsification for removal of cataract involves a number of steps, and is typically performed under an operating microscope. Each footstep must exist carefully and skillfully performed in order to attain the desired result. The steps may exist described as follows:
- Anaesthesia; Topical anesthetic agents are most usually used and may be placed on the globe prior to surgery and or in the globe during surgery.[12] Anesthetic injection techniques include sub-conjunctival injections and or injections posterior to the globe (retrobulbar block) to produce a regional nerve block. Intravenous sedation may be combined with the topical and injection techniques. Full general anesthesia with the patient unconscious from intravenous agents and or inhaled gases is another technique, however general anaesthetic is non the standard treatment.
- Exposure of the eyeball using an eyelid speculum;
- Entry into the eye through a minimal incision (corneal or scleral);
- Viscoelastic This is injected to stabilize the anterior chamber, to aid maintain heart pressurization, and to distend the cataract'south sheathing during IOL implantation.
- Capsulorhexis; This pace involves making a circular opening on the front surface of the lens in order to access the cloudy lens material within.
- Hydrodissection; The cataract'due south outer cortical layer is dissected, by the injection of a fluid wave, from the sheathing, the outer-nearly skin of the cataract.
- Hydrodelineation; The cataract's outer softer epi-nucleus is separated from the inner firmer endo-nucleus by the injection of a fluid wave. The epi-nucleus serves to protect the cataract'south capsule during phacoemulsification of the endo-nucleus.
- Ultrasonic destruction or emulsification of the cataract after nuclear cracking or chopping (if needed), careful aspiration of the remaining lens cortex (outer layer of lens) fabric from the capsular bag, capsular polishing (if needed);
- Implantation of the, ordinarily foldable, intraocular lens (IOL);
- Viscoelastic removal; The viscoelastic injected to stabilize the anterior chamber, protect the cornea from damage, and distend the cataract's capsule during IOL implantation must exist removed from the eye to prevent viscoelastic glaucoma (a severe intra-ocular force per unit area increment) post-operatively. This is washed via suction from the irrigation-aspiration instrument.
- Wound sealing / hydration (if needed). The incision is sealed past elevating the pressure level inside the globe which presses the internal tissue against the external tissue of the incision forcing closed the incision.
The educatee is dilated using drops (if the IOL is to be placed behind the iris) to help improve visualise the cataract. Educatee-constricting drops are reserved for secondary implantation of the IOL in forepart of the iris (if the cataract has already been removed without master IOL implantation). Anesthesia may be placed topically (eyedrops) or via injection next to (peribulbar) or behind (retrobulbar) the eye.[12] Topical anaesthetics are normally used at the same time every bit a intracameral lidocaine injection to reduce hurting during the performance.[12] Oral or intravenous sedation may also be used to reduce anxiety. General anesthesia is rarely necessary, simply may be employed for children and adults with particular medical or psychiatric issues.[12] The operation may occur on a stretcher or a reclining exam chair. The eyelids and surrounding skin will be swabbed with disinfectant. The face is covered with a cloth or sheet, with an opening for the operative eye. The eyelid is held open with a speculum to minimize blinking during surgery. Hurting is ordinarily minimal in properly anesthetised eyes, though a pressure sensation and discomfort from the bright operating microscope light is common. The ocular surface is kept moist using sterile saline eye drops or methylcellulose viscoelastic. The discission into the lens of the centre is performed at or nearly where the cornea and sclera see (limbus = corneoscleral junction). Advantages of the smaller incision include use of few or no stitches and shortened recovery time.[iv] [xiii]
A capsulotomy (rarely known equally cystotomy) is a process to open a portion of the lens capsule, using an musical instrument called a cystotome.[fourteen] An inductive capsulotomy refers to the opening of the front portion of the lens capsule, whereas a posterior capsulotomy refers to the opening of the back portion of the lens capsule. In phacoemulsification, the surgeon performs an inductive continuous curvilinear capsulorhexis, to create a round and smooth opening through which the lens nucleus tin be emulsified and the intraocular lens implant inserted.
Following cataract removal (via ECCE or phacoemulsification, as described in a higher place), an intraocular lens is usually inserted. Afterward the IOL is inserted, the surgeon checks that the incision does not leak fluid. This is a very important step, since wound leakage increases the adventure of unwanted microorganisms gaining access into the centre and predisposing it to endophathalmitis. An antibiotic/steroid combination middle drop is put in and an center shield may be practical on the operated eye, sometimes supplemented with an center patch.
Antibiotics may exist administered pre-operatively, intra-operatively, and/or mail service-operatively. Frequently a topical corticosteroid is used in combination with topical antibiotics post-operatively.
Most cataract operations are performed under a local anaesthetic, allowing the patient to go home the aforementioned day. The utilize of an middle patch may be indicated, usually for about some hours, later which the patient is instructed to start using the eyedrops to command the inflammation and the antibiotics that prevent infection. Lens and cataract procedures are commonly performed in an outpatient setting; in the United states of america, 99.nine% of lens and cataract procedures were done in an convalescent setting in 2012.[xv]
Occasionally, a peripheral iridectomy may be performed to minimize the adventure of pupillary block glaucoma. An opening through the iris can be fashioned manually (surgical iridectomy) or with a laser (called Nd-YAG light amplification by stimulated emission of radiation iridotomy). The laser peripheral iridotomy may exist performed either prior to or post-obit cataract surgery.
The iridectomy hole is larger when done manually than when performed with a light amplification by stimulated emission of radiation. When the transmission surgical procedure is performed, some negative side-effects may occur, such as that the opening of the iris tin can be seen by others (aesthetics), and the calorie-free can fall into the middle through the new hole, creating some visual disturbances. In the case of visual disturbances, the eye and brain oft learn to compensate and ignore the disturbances over a couple of months. Sometimes the peripheral iris opening can heal, which means that the pigsty ceases to exist. This is the reason that the surgeon sometimes makes two holes, and then that at least one hole is kept open up.
After the surgery, the patient is instructed to use anti-inflammatory and antibiotic eye-drops for upwardly to two weeks (depending on the inflammation status of the eye and some other variables). The eye surgeon volition estimate, based on each patient's idiosyncrasies, the time length to apply the eye drops. The eye will exist mostly recovered within a calendar week, and complete recovery should be expected in about a calendar month. The patient should not participate in contact/extreme sports until cleared to practise so by the center surgeon.
Complications [edit]
Complications after cataract surgery are relatively uncommon.
- PVD – Posterior vitreous disengagement does not straight threaten vision. Even so, it is of increasing involvement because the interaction between the vitreous body and the retina might play a decisive role in the development of major pathologic vitreoretinal conditions. PVD may be more than problematic with younger patients, since many patients older than sixty have already gone through PVD. PVD may be accompanied past peripheral low-cal flashes and increasing numbers of floaters.

Slit lamp photo of IOL showing Posterior capsular opacification (PCO) visible a few months later implantation of Intraocular lens in middle, seen on retroillumination
- PCO – Some people can develop a posterior capsular opacification (PCO), besides called an later-cataract. Every bit a physiological change expected later on cataract surgery, the posterior capsular cells undergo hyperplasia and cellular migration, showing up as a thickening, opacification and clouding of the posterior lens capsule (which is left behind when the cataract was removed, for placement of the IOL). This may compromise visual vigil and the ophthalmologist can utilise a device to correct this state of affairs. It can be safely and painlessly corrected using a laser device to make small holes in the posterior lens sheathing of the crystalline. Information technology usually is a quick outpatient process that uses a Nd-YAG light amplification by stimulated emission of radiation (neodymium-yttrium-aluminum-garnet) to disrupt and clear the central portion of the opacified posterior pole of the capsule (posterior capsulotomy).[sixteen] This creates a clear central visual axis for improving visual acuity.[17] In very thick opacified posterior capsules, a surgical (manual) capsulectomy is the surgical procedure performed. A YAG capsulotomy is, however, a factor which must be taken in consideration in the event of IOL replacement every bit vitreous can drift toward the anterior chamber through the opening hitherto occluded past the IOL.
- Posterior capsular tear may be a complication during cataract surgery. The rate of posterior capsular tear among skilled surgeons is around 2% to 5%. It refers to a rupture of the posterior sheathing of the natural lens. Surgical management may involve anterior vitrectomy and, occasionally, alternative planning for implanting the intraocular lens, either in the ciliary sulcus, in the anterior chamber (in front of the iris), or, less commonly, sutured to the sclera.
- Retinal detachment normally occurs at a prevalence of 1 in one,000 (0.1%), but patients who have had cataract surgery are at an increased risk (0.5–0.6%) of developing rhegmatogenous retinal detachment (RRD) – the most common grade of retinal detachment.[xviii] Cataract surgery speeds upward the rate of vitreous sense of humour liquefaction and this leads to increased rates of RRD.[xix] When a retinal tear occurs, vitreous liquid enters the space between the retina and retinal pigmented epithelium (RPE) and presents as flashes of lite (photopsia), dark floaters, and loss of peripheral vision.[18]
- Toxic Anterior Segment Syndrome or TASS is a non-infectious inflammatory condition that may occur following cataract surgery. Information technology is usually treated with topical corticosteroids in high dosage and frequency.
- Endophthalmitis is a serious infection of the intraocular tissues, usually following intraocular surgery, or penetrating trauma. There is some business concern that the articulate cornea incision might predispose to the increase of endophthalmitis but in that location is no conclusive written report to corroborate this suspicion.[twenty] An intracameral injection of antibiotics may exist used as a preventive measure.
- Glaucoma may occur and information technology may be very hard to control. Information technology is ordinarily associated with inflammation, specially when trivial fragments or chunks of the nucleus get access to the vitreous cavity. Some experts recommend early intervention when this condition occurs (posterior pars plana vitrectomy). Neovascular glaucoma may occur, specially in diabetic patients. In some patients, the intraocular pressure may remain and then high that blindness may ensue.
- Swelling or edema of the central part of the retina, called macula, resulting in macular edema, tin can occur a few days or weeks later on surgery. Most such cases can be successfully treated. Preventative utilise of nonsteroidal anti-inflammatory drugs has been reported to reduce the chance of macular edema to some extent.[21]
- Uveitis–Glaucoma–Hyphema syndrome: This is a complication of cataract surgery acquired due to the mechanical irritation of mispositioned intraocular lens over iris, ciliary body or iridocorneal bending.[22]
- Other possible complications include: Swelling or edema of the cornea, sometimes associated with cloudy vision, which may be transient or permanent (pseudophakic bullous keratopathy). Displacement or dislocation of the intraocular lens implant may rarely occur. Unplanned high refractive error (either myopic or hypermetropic) may occur due to error in the ultrasonic biometry (measure of the length and the required intraocular lens ability). Cyanopsia, in which the patient sees everything tinted with blueish, often occurs for a few days, weeks or months later on removal of a cataract. Floaters commonly announced afterwards surgery.
History [edit]
Ancient Babylonia [edit]
Cataract surgery was first mentioned in the Babylonian code of Hammurabi 1750BCE.[23]
Ancient Egypt [edit]
Possibly the starting time delineation of cataract surgery in recorded history is on a statue from the 5th Dynasty (2467–2457BCE).[24] It is further declared that a "relief painting from tomb number TT 217 in a worker settlement in Deir-el-Medina" shows "the man buried in the tomb, Ipuy,... one of the builders of royal tombs in the renowned Valley of the Kings, circa 1279–1213 BC"[25] every bit he underwent cataract surgery.[24]
Ancient Greece [edit]
Galen of Pergamon 2nd centuryCE, a prominent Greek physician, surgeon and philosopher, performed an performance similar to modern cataract surgery. Using a needle-shaped instrument, Galen attempted to remove a cataract-affected lens.[26] [27] Although many 20th century historians have claimed that Galen believed the lens to be in the exact center of the center, Galen actually understood that the crystalline lens is located in the anterior aspect of the human eye.[28]
India [edit]
A form of cataract surgery, now known as "couching", was found in ancient India and subsequently introduced to other countries by the Indian physician Sushruta (c. 6th century BCE),[29] who described it in his work the Compendium of Sushruta or Sushruta Samhita. The Uttaratantra section of the Compendium, chapter 17, verses 55–69, describes an operation in which a curved needle was used to push the opaque phlegmatic affair (kapha in Sanskrit) in the eye out of the style of vision. The phlegm was so blown out of the nose. The center would later be soaked with warm clarified butter and then bandaged. Here is translation from the original Sanskrit:
vv. 55–56: At present process of surgical functioning of ślaiṣmika liṅganāśa (cataract) will be described. It should be taken up (for treatment) if the diseased portion in the pupillary region is non shaped like one-half moon, sweat driblet or pearl: not fixed, uneven and thin in the centre, streaked or variegated and is not found painful or reddish.
vv. 57–61ab: In moderate season, after unction and sudation, the patient should be positioned and held firmly while gazing at his nose steadily. At present the wise surgeon leaving two parts of white circumvolve from the black one towards the outer canthus should open up his eyes properly costless from vascular network and so with a barley-tipped rod-similar instrument held firmly in hand with heart, alphabetize and thumb fingers should puncture the natural hole-similar indicate with effort and confidence non below, above or in sides. The left centre should be punctured with correct hand and vice-versa. When punctured properly a drib of fluid comes out and alsoe there is some typical sound.
vv. 61bc–64ab: Just after puncturing, the expert should irrigate the heart with breast-milk and foment information technology from outside with vāta-[wind-]alleviating tender leaves, irrespective of doṣa [defect] being stable or mobile, belongings the instrument properly in position. And then the pupillary circle should be scraped with the tip of the musical instrument while the patient, closing the nostril of the side reverse to the punctured heart, should accident so that kapha [phlegm] located in the region be eliminated.
vv. 64cd–67: When pupillary region becomes clear similar cloudless sun and is painless, it should be considered every bit scraped properly. (If doṣa [defect] cannot be eliminated or information technology reappears, puncturing is repeated later unction and sudation.) When the sights are seen properly the śalākā [probe] should be removed slowly, eye all-powerful with ghee and bandaged. Then the patient :should lie downward in supine position in a peaceful bedroom. He should avoid belching, cough, sneezing, spitting and shaking during the operation and thereafter should detect the restrictions as after intake of sneha [oil].
5. 68: Eye should be washed with vāta-[wind-]alleviating decoctions after every three days and to eliminate fear of (aggravation of) vāyu [current of air], it should besides be fomented every bit mentioned before (from outside and mildly).
v. 69: After observing restrictions for 10 days in this way, post-operative measures to normalise vision should be employed along with low-cal diet in proper quantity.[thirty]
The removal of cataracts by surgery was also introduced into China from India, and flourished in the Sui (581–618CE) and Tang dynasties (618–907CE).[31]
West Africa [edit]
The removal of cataracts was a common surgical procedure in Djenné[32](equally in many other parts of Africa[33]).
Europe and the Islamic world [edit]
The first references to cataract and its treatment in Europe are found in 29 AD in De Medicinae, the work of the Latin encyclopedist Aulus Cornelius Celsus, which also describes a couching operation.[ citation needed ]
Couching continued to exist used throughout the Middle Ages and is still used in some parts of Africa and in Yemen.[34] Nonetheless, couching is an ineffective and dangerous method of cataract therapy, and often results in patients remaining bullheaded or with only partially restored vision.[34] For the most office, it has now been replaced by extracapsular cataract surgery and, especially, phacoemulsification.[35]
The lens tin can also exist removed past suction through a hollow instrument. Statuary oral suction instruments accept been unearthed that seem to have been used for this method of cataract extraction during the second centuryCE.[36] Such a procedure was described by the tenth-century Persian dr. Muhammad ibn Zakariya al-Razi, who attributed it to Antyllus, a 2d-century Greek physician. The process "required a large incision in the eye, a hollow needle, and an assistant with an extraordinary lung capacity".[37] This suction procedure was also described by the Iraqi ophthalmologist Ammar Al-Mawsili, in his Choice of Eye Diseases, as well written in the tenth century.[37] He presented example histories of its utilize, claiming to have had success with it on a number of patients.[37] Extracting the lens has the benefit of removing the possibility of the lens migrating back into the field of vision.[38] A later variant of the cataract needle in 14th-century Egypt, reported by the oculist Al-Shadhili, used a spiral to produce suction. It is not clear, notwithstanding, how frequently this method was used every bit other writers, including Abu al-Qasim al-Zahrawi and Al-Shadhili, showed a lack of experience with this process or claimed it was ineffective.[37] [ verification needed ]
Eighteenth century and later [edit]
In 1748, Jacques Daviel was the start modern European doc to successfully excerpt cataracts from the eye. In America, an early on form of surgery known as cataract couching may have been performed in 1611,[39] and cataract extraction was most likely performed by 1776.[forty] Cataract extraction by aspiration of lens material through a tube to which suction is practical was performed by Philadelphia surgeon Philip Syng Physick in 1815.[41]
King Serfoji Two Bhonsle of Thanjavur in Republic of india performed cataract surgeries as documented in manuscripts at the Saraswathi Mahal Library in the early 1800s.[ citation needed ]
In 1949, Harold Ridley introduced the concept of implantation of the intraocular lens which permitted more than efficient and comfortable visual rehabilitation possible later cataract surgery.[42]
In 1967, Charles Kelman introduced phacoemulsification, a technique that uses ultrasonic waves to emulsify the nucleus of the crystalline lens in gild to remove the cataracts without a large incision. This new method of surgery decreased the need for an extended hospital stay and fabricated the surgery ambulatory. Patients who undergo cataract surgery hardly complain of pain or even discomfort during the procedure. Withal patients who have topical anesthesia, rather than peribulbar cake anesthesia, may experience some discomfort.[ citation needed ]
According to surveys of members of the American Society of Cataract and Refractive Surgery, approximately 2.85 million cataract procedures were performed in the United States during 2004 and 2.79 one thousand thousand in 2005.[43]
In Republic of india, modern surgery with intraocular lens insertion in government- and NGO-sponsored Heart Surgical camps has replaced older surgical procedures.[ citation needed ] In rare cases, infections have caused blindness among some of the patients in mass free eye camps in India.[44]
Usage in the United Kingdom [edit]
In the UK the practice of the various National Health Service healthcare providers in referring people with cataracts to surgery varied widely as of 2017, with many of the providers only referring people with moderate or severe vision loss, and often with delays.[45] This is despite guidance issued by the NHS executive in 2000 urging providers to standardize intendance, streamline the process, and increase the number of cataract surgeries performed in social club to come across the needs of the aging population.[46] The national ophthalmology outcomes inspect in 2019 found five NHS trusts with complication rates between i.5% and ii.one%, but since the first national cataract audit in 2010, at that place had been a 38% reduction in posterior capsule rupture complications.[47]
See also [edit]
- Africa Cataract Project
- Eye surgery
- Himalayan Cataract Projection
References [edit]
- ^ "Cataracts | National Heart Institute". www.nei.nih.gov . Retrieved 2020-07-27 .
- ^ "Cataract surgery". Mayo Foundation for Medical Teaching and Research (MFMER) . Retrieved nineteen July 2021.
- ^ Lawrence, David; Fedorowicz, Zbys; van Zuuren, Esther J (2015-eleven-02). Cochrane Eyes and Vision Group (ed.). "Solar day care versus in-patient surgery for age-related cataract". Cochrane Database of Systematic Reviews (xi): CD004242. doi:10.1002/14651858.CD004242.pub5. PMC7197209. PMID 26524611.
- ^ a b c Extracapsular Cataract Extraction – Definition, Purpose, Demographics, Description, Diagnosis/preparation, Aftercare, Risks, Normal results, Morbidity and mortality rates, Alternatives Encyclopedia of Surgery: A Guide for Patients and Caregivers
- ^ Alió JL, Abdou AA, Puente AA, Zato MA, Nagy Z (June 2014). "Femtosecond light amplification by stimulated emission of radiation cataract surgery: updates on technologies and outcomes". Journal of Refractive Surgery. 30 (6): 420–427. doi:10.3928/1081597x-20140516-01. PMID 24972409.
- ^ Popovic 1000, Campos-Möller X, Schlenker MB, Ahmed II (October 2016). "Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: A Meta-Analysis of 14 567 Optics". Ophthalmology. 123 (ten): 2113–2126. doi:10.1016/j.ophtha.2016.07.005. PMID 27538796.
- ^ "Cryotherapy for cataracts". Encyclopedia of Surgery
- ^ Meadow, Norman B. "Cryotherapy: A fall from grace, simply not a crash". Ophthalmology Times. October 15, 2005.
- ^ New Device Blessing – CrystaLens Model AT-45 All-around IOL – P030002. U.S. Food and Drug Administration.
- ^ Charters, Linda Anticipation is cardinal to managing intra-operative floppy iris syndrome Archived 2006-ten-22 at the Wayback Machine. Ophthalmology Times. June 15, 2006.
- ^ Keay L, Lindsley 1000, Tielsch J, Katz J, Schein O (January 2019). "Routine preoperative medical testing for cataract surgery". The Cochrane Database of Systematic Reviews. 1: CD007293. doi:10.1002/14651858.CD007293.pub4. PMC6353242. PMID 30616299.
- ^ a b c d Minakaran, Neda; Ezra, Daniel G; Allan, Bruce DS (2020-07-28). "Topical anaesthesia plus intracameral lidocaine versus topical anaesthesia alone for phacoemulsification cataract surgery in adults". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd005276.pub4. ISSN 1465-1858. PMC8190979.
- ^ Surgery Encyclopedia – Phacoemulsification for cataracts
- ^ Capsulorhexis using a cystotome needle during cataract surgery Archived 2008-08-26 at the Wayback Car
- ^ Wier LM, Steiner CA, Owens PL (February 2015). "Surgeries in Infirmary-Owned Outpatient Facilities, 2012". HCUP Statistical Brief #188. Rockville, Dr.: Bureau for Healthcare Research and Quality.
- ^ "Videos: YAG Laser Capsulotomy". Pacific Cataract and Laser Institute . Retrieved ii April 2019.
- ^ Surgery Encyclopedia – Light amplification by stimulated emission of radiation posterior capsulotomy
- ^ a b Steel, David (2014-03-03). "Retinal disengagement". BMJ Clinical Evidence. 2014. ISSN 1752-8526. PMC3940167. PMID 24807890.
- ^ Feltgen, Nicolas; Walter, Peter (2014-01-06). "Rhegmatogenous retinal detachment – an ophthalmologic emergency". Deutsches Ärzteblatt International. 111 (one–2): 12–21, quiz 22. doi:x.3238/arztebl.2014.0012. ISSN 1866-0452. PMC3948016. PMID 24565273.
- ^ "Endophthalmitis". The Lecturio Medical Concept Library . Retrieved 19 July 2021.
- ^ Lim BX, Lim CH, Lim DK, Evans JR, Bunce C, Wormald R (November 2016). "Condom non-steroidal anti-inflammatory drugs for the prevention of macular oedema subsequently cataract surgery". The Cochrane Database of Systematic Reviews. 11: CD006683. doi:10.1002/14651858.CD006683.pub3. PMC6464900. PMID 27801522.
- ^ Zemba, Mihail; Camburu, Georgiana (2017). "Uveitis–Glaucoma–Hyphaema Syndrome. General review". Romanaian Journal of Ophthalmology. 61 (i): xi–17. doi:ten.22336/rjo.2017.three. ISSN 2457-4325. PMC5710046. PMID 29450365.
- ^ Ascaso, Francisco J.; Lizana, Joaquín; Cristóbal, José A. (March 2009). "Cataract surgery in aboriginal Egypt". Journal of Cataract & Refractive Surgery. 35 (3): 607–608. doi:10.1016/j.jcrs.2008.11.052. ISSN 0886-3350. PMID 19251160.
- ^ a b . doi:10.1016/j.jcrs.2008.eleven.052. ;
- ^ "Hoax: Picture from Ancient Arab republic of egypt Nada to Practice with COVID-19 Examination". TASR. 25 January 2021.
- ^ Urabe H (September 1976). "[Classification of ringworm infections (author's transl)]". Nihon Hifuka Gakkai Zasshi. The Japanese Periodical of Dermatology. 86 (10): 573–581. PMID 1034789.
- ^ Lois N. Magner (1992). A History of Medicine. CRC Press. p. 91.
- ^ Leffler CT, Hadi TM, Udupa A, Schwartz SG, Schwartz D (2016). "A medieval fallacy: the crystalline lens in the center of the centre". Clinical Ophthalmology. 10 (x): 649–662. doi:ten.2147/OPTH.S100708. PMC4833360. PMID 27114699.
- ^ Meulenbeld, G. January (1999–2002). A History of Indian Medical Literature. Groningen: Forsten.
- ^ Sharma, Priya Vrat (2001). Suśruta-Saṃhitā with English language translation of text and Ḍalhaṇa'south commentary along with disquisitional notes. Vol ĪI (Kalpasthāna and Uttaratantra). Varanasi, India: Chaukhambha Visvabharati Oriental. pp. 202–204.
- ^ Deshpande, Vijaya (2000). "Ophthalmic surgery: a chapter in the history of Sino-Indian medical contacts". Message of the School of Oriental and African Studies. 63 (3): 370–388. doi:10.1017/S0041977X00008454. S2CID 162655091. See also Deshpande, Vijaya (1999). "Indian influences on early Chinese ophthalmology: glaucoma as a case report". Bulletin of the School of Oriental and African Studies. 62 (22): 306–322. doi:x.1017/S0041977X00016724.
- ^ McKissack, Patricia; McKissack, Fredrick (1995). The Majestic Kingdoms of Ghana, Mali, and Songhay Life in Medieval Africa. Macmillan. p. 104. ISBN978-0-8050-4259-seven.
- ^ Thomson, Ethel (1965). "Primitive African Medical Lore and Witchcraft". Bulletin of the Medical Library Association. 53: 89–ninety. ISSN 0025-7338. PMC198231. PMID 14223742.
- ^ a b 'Couching' for cataracts remains a persistent problem in Yemen Archived 2011-07-26 at the Wayback Machine, EuroTimes, September 2005, p. 11.
- ^ "Toric Lens Implants | Pacific Cataract and Laser Institute: For Doctors of Optometry". odpcli.com . Retrieved 2019-10-09 .
- ^ Bergman William C (2009). "Factors influencing the genesis of neurosurgical technology". Neurosurgical Focus. 27 (3): E3. doi:x.3171/2009.6.FOCUS09117. PMID 19722817. .
- ^ a b c d Brutal-Smith Due east (Baronial 2000). "The practice of surgery in Islamic lands: myth and reality". Social History of Medicine. 13 (2): 307–321. doi:10.1093/shm/thirteen.2.307. PMID 14535259.
- ^ Finger, Stanley (1994). Origins of Neuroscience: A History of Explorations Into Brain Function. Oxford Academy Press. p. 70. ISBN978-0-xix-514694-3.
- ^ Leffler CT, Wainsztein RD (2016). "The first cataract surgeons in Latin America: 1611–1830". Clinical Ophthalmology. 10: 679–694. doi:10.2147/OPTH.S105825. PMC4841434. PMID 27143845.
- ^ Leffler CT, Schwartz SG, Grzybowski A, Braich PS (2015). "The first cataract surgeons in Anglo-America". Survey of Ophthalmology. 60 (1): 86–92. doi:ten.1016/j.survophthal.2014.08.002. PMC4262555. PMID 25444521.
- ^ Leffler CT, Letocha CE, Pierson K, Schwartz SG (2017). "Aspiration of cataract in 1815 in Philadelphia, Pennsylvania". Digital Journal of Ophthalmology. 23 (four): 4–7. doi:ten.5693/djo.01.2017.x.001. PMC5791631. PMID 29403333.
- ^ Davis, 1000. (January 2016). "The Evolution of Cataract Surgery". Missouri Medicine. Missouri Country Medical Association. 113 (1): 58–62. PMC6139750. PMID 27039493.
- ^ American Academy of Ophthalmology reference [ permanent expressionless link ]
- ^ "India cataracts scandal: Arrests over 'botched' surgery". BBC. 5 Dec 2014.
- ^ "Two thirds of middle units restricting access to cataract surgery". OnMedica. ten November 2017. Retrieved 28 December 2017.
- ^ "Activeness on Cataracts Good Exercise Guidance" (PDF). NHS Executive via the Royal Higher of Ophthalmologists. January 2000. , referenced in "Context: Guideline for Cataracts in adults". Dainty. October 2017.
- ^ "Revealed: The trusts with the highest cataract complexity rates". Health Service Journal. xi Oct 2019. Retrieved 21 November 2019.
Further reading [edit]
- Finger, Stanley (2001). Origins of Neuroscience: A History of Explorations Into Brain Function. Oxford University Press. ISBN978-0-19-514694-3.
- Lade, Arnie; Svoboda, Robert (2000). Chinese Medicine and Ayurveda. Motilal Banarsidass. ISBN978-81-208-1472-ane.
- Frampton, Geoff; Harris, Petra; Cooper, Keith; Lotery, Andrew; Shepherd, Jonathan (2014). "The clinical effectiveness and toll-effectiveness of second-center cataract surgery: a systematic review and economic evaluation". Health Engineering science Cess. Southampton United kingdom of great britain and northern ireland: NIHR Journals Library. 18 (68): 1–205, v–vi. doi:10.3310/hta18680. PMC4781176. PMID 25405576. 18.68.
- Prajna, N. Venkatesh; Ravilla, Thulasiraj D.; Srinivasan, Sathish (2015). "Ch: 11. Cataract Surgery". In Debas, H.T.; Donkor, P.; Gawande, A.; Jamison, D.T.; Kruk, M.Eastward.; Mock, C.N. (eds.). Essential Surgery. Disease Control Priorities. Vol. 1 (third ed.). The International Bank for Reconstruction and Development / The World Bank. ISBN978-1-4648-0346-viii.
External links [edit]
- Cataract Surgery – slideshow by The New York Times
Source: https://en.wikipedia.org/wiki/Cataract_surgery
0 Response to "Caterack Removal"
Post a Comment